-
胆囊癌是中国最常见的胆道系统恶性肿瘤,其5年生存率只有5%左右[1]。根治性切除目前仍是胆囊恶性肿瘤的主要治疗方法。T2期胆囊癌是指癌组织侵犯肌层结缔组织深层但未穿透浆膜层。中国《胆囊良性疾病外科治疗的专家共识(2021版)》建议对T2期胆管肿瘤进行肝楔形切除或4b/5切除[1]。美国国立综合癌症网络(NCCN)指南建议对T2期的胆囊癌行4b段以及5段切除,同时行扩大的肝切除,门淋巴结的清扫或胆管的切除[2]。但有研究发现,T2期胆囊癌患者行肝楔形切除或4b/5切除与单纯胆囊切除手术相比,生存期没有显著差异[3]。因此,本研究皆在比较不同手术范围对于T2期胆囊癌患者预后的影响。
-
1 资料与方法
-
1.1 检索策略
-
检索数据库包括 Pubmed、Embase、Web of Science、Cochrane Library、中国知网、万方数据库以及维普数据库。检索时限均从建库至2022年12月,语种为英文或中文。英文检索词汇包括:gallbladder carcinoma,surgery,cholecystectomy,radical cholecystectomy,hepatectomy,liver resection。中文检索词汇包括:胆囊癌、手术、胆囊切除术、根治性胆囊切除、肝切除。
-
1.2 纳人与排除标准
-
纳入标准:1)入选病例均为术后病理分期证实为T2期胆囊癌。2)治疗过程进行了肝切除术与非肝切除术之间的比较。3)报道了手术后的早期不良事件,其中包括:术后30d内的死亡率,与外科有关的并发症(胆漏、肝功能衰竭、胆瘘、腹水等),一般并发症(吻合口瘘、伤口感染、脓肿、肠梗阻、急性肾衰竭、尿路感染、妄、呼吸及心血管并发症)。4)报道长期预后,例如总体生存率或无病生存率。排除标准:1)仅为单种术式的研究;2)纽卡斯尔-渥太华量表(newcastle-ottawa scale,NOS)评分<4; 3)临床资料数据不完备;4)综述以及个案报道; 5)不能获得完整的文本。
-
1.3 文献筛选及数据提取
-
两名研究人员按照规范分别对文献进行筛选和抽取,当出现分歧时,将由两名研究人员共同商讨。数据抽取的主要内容有:第一作者、发表时间、国家、样本量、年龄、性别等,手术方法及评估指标等。
-
1.4 文献质量评价
-
以NOS量表为依据,对文献进行质量评价,评价标准包括研究人群选择、组间可比性及结果测量。评分0~9 分,6分及以上为高质量研究,小于6分为低质量研究。
-
1.5 评价指标
-
Meta 分析评价指标包括:术后总体生存率、术后无病生存率、术后并发症发生率及术后30 d内死亡率。
-
1.6 数据处理
-
采用RevMan5.4软件进行统计分析。在文献异质化研究中,若12≥ 50%,以随机效应模型对文献进行整合,若12<50%,以固定效应模型对文献进行整合。结果以危险比(RR)及95%置信区间(CI)展示,P<0.05为差异有统计学意义。
-
2 结果
-
2.1 文献检索结果
-
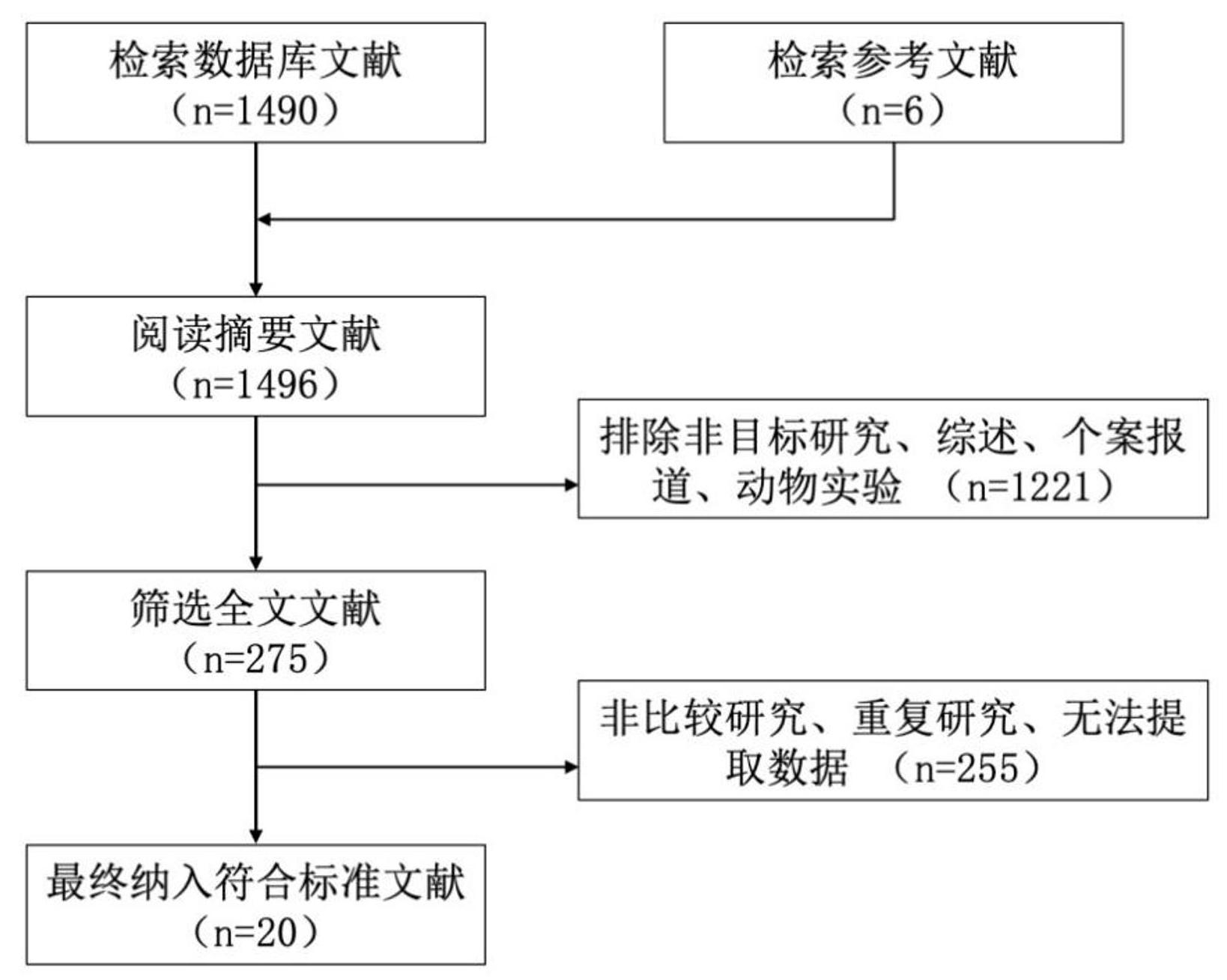
通过检索不同数据库,最终纳入符合标准的相关文献 20 篇[4-23]。所有研究均为回顾性队列研究。最终共纳人患者3222例,其中单纯胆囊切除患者1263例(非肝切除组),胆囊切除联合肝切除患者1959例(肝切除组)。文献筛选流程详见图1。
-
图1 文献筛选流程
-
2.2 质量评价及发表偏倚
-
文献均为 1992 年一2022年的回顾性研究,其中中国1篇,美国3篇,日本5篇,韩国11篇。纳入的20篇文献质量均评价为高质量,具体详见表1。漏斗图分析显示,两者术后并发症两侧结果不完全对称,原因可能是存在发表偏倚,具体详见图2。
-
2.3 术后总生存率
-
18篇文献报道了两组患者术后总生存率,I2=75%,提示文献间存在较大异质性,采用随机效应模式对相关的研究进行了整合。研究发现,两组患者的总体生存率无统计学差异(RR=0.93,95%CI:0.77~1.12,P=0.44),见图3。
-
2.4 术后无病生存率
-
6篇文献报道了两组患者术后无病生存率,12=60%,提示文献间存在较大异质性,采用随机效应模型对相关的文献进行了整合。结果表明,两组患者的无病生存率无统计学差别(RR=1.11,95%CI:0.84~1.47,P=0.45),见图4。
-
2.5 术后并发症发生率
-
有5篇文献报道了两组患者术后并发症的发生率,12=51%,提示文献间存在较大异质性,采用随机效应模型对相关的文献进行了整合。结果显示两组患者术后并发症发生率无显著统计学差异(RR=2.00,95%CI:0.71~5.62,P=0.19)见图5。
-
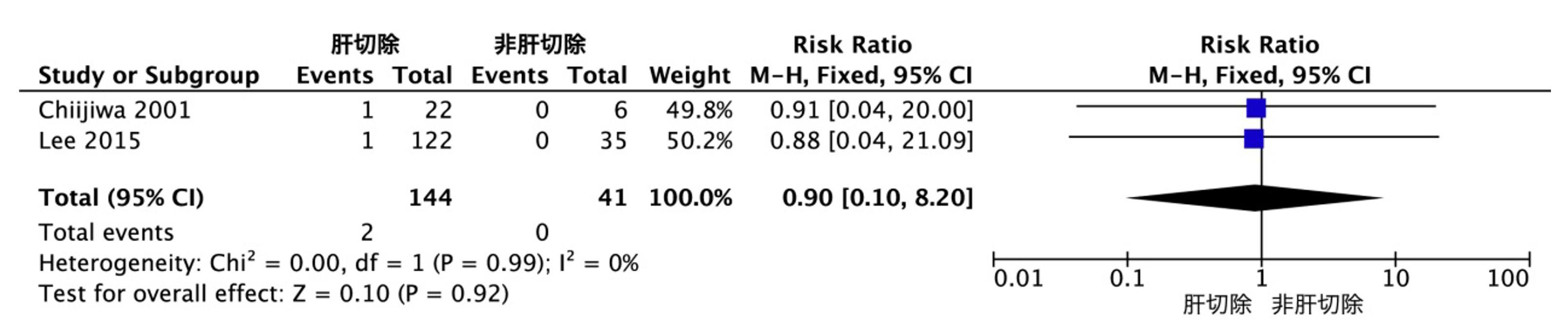
2.6 术后30 d内死亡率
-
2 篇纳人文献报道了两组患者术后无病生存率,I2=0%,提示文献间无异质性,采用固定的效应模型来整合相关的文献。结果显示,两组患者术后30 d内死亡率无统计学差异RR=0.90,95%CI:0.10~8.02,P=0.92),见图6。
-
注:OS为总生存时间; DFS为无进展生存时间
-
图2 文献发表偏倚分析漏斗图
-
图3 两组患者术后总生存率比较森林图
-
图4 两组患者术后无病生存率比较森林图
-
图5 两组患者术后并发症率比较森林图
-
图6 两组患者术后 30 d 内死亡率比较森林图
-
3 讨论
-
目前,外科治疗T2期胆囊癌的切除范围尚有争论。第8版美国癌症联合委员会(AJCC)胆囊癌TNM分期根据病灶部位将T2期胆囊癌分为T2a期(腹腔侧)和 T2b 期(肝脏侧)[24]。而有研究表明,T2a及 T2b 期患者的预后有明显的差异[16,25]。T2a期瘤体并不邻近肝脏组织,侵袭肝的可能性较小,其争议点主要在于是否需要联合肝切除。而由于胆囊肝脏侧无浆膜层,并有密集的血管淋巴管组织,T2b期肿瘤更易侵犯肝脏组织,因此其争议点主要在于肝脏切除的范围。鉴于肝楔形切除并不会增加手术难度,《胆囊良性疾病外科治疗的专家共识(2021版)》推荐T2期胆囊癌均应行肝楔形切除或4b/5段切除术[1]。多项研究显示,肝切除术可改善胆囊癌T2b期患者的预后,而T2a期患者并不能从中获益[25-27]。本研究显示,对于T2期胆囊癌患者,肝切除组与非肝切除组相比在术后长期生存率、围手术期并发症和死亡率方面均无显著统计学差异。由于T2期肿瘤没有侵犯到浆膜组织,肝切除是为了获得胆囊癌的阴性切缘,因此这一结论似乎是合理的。所以术前精确地确定肿瘤浸润深度是决定手术切除范围的关键。虽然常规腹部超声和CT已广泛用于术前分期,但其对于肿瘤的浸润程度的评估,远不及内镜和腹腔镜。腹腔镜具有更高的分辨率图像,因此能够更好地显示胆囊壁的多层结构,更有助于选择合理的术式并改善患者预后[28]。如果肿瘤深度仅限于肌层周围结缔组织,或者如果术中冰冻切片分析确认胆囊在肝侧的显微镜阴性切缘,则可能不需要行肝切除。对于在简单胆囊切除术后病理报告中被诊断出胆囊癌的患者,如果标本的肝侧和胆囊管切缘均为癌细胞阴性,则可能不需要进一步行肝脏切除。
-
本研究的局限性包括:所有纳入研究均采用了回顾性设计,可能存在选择偏倚和其他混杂因素,特别是东西方国家治疗胆囊癌的差异性,因此还需进行前瞻性的随机对照试验(RCT)研究来验证。此外,由于样本的差异性,针对胆囊癌根治术重要组成部分区域淋巴结清扫范围,无法进一步分析联合以上两种术式评判两者之间差异,此外,关于血管侵犯以及术后化疗等异质性的文献并未纳人本项研究。
-
综上所述,本研究显示对于T2期胆囊癌,行肝切除术对于患者的围手术期及远期预后无显著影响。如果术前评估确认肿瘤深度仅限于肌层周围结缔组织,并且术中冰冻切片确认显微镜阴性切缘,则T2期胆囊癌可能不需要联合肝切除术。类似地,对于在单纯胆囊切除术后意外诊断为胆囊癌的患者,可能不需要进一步的肝切除。因为大部分的研究都是回顾性的,所以这些结论还有待于前瞻性RCT研究来证实。
-
参考文献
-
[1] 中华医学会外科学分会胆道外科学组,中国医师协会外科医师分会胆道外科医师委员会.《胆囊良性疾病外科治疗的专家共识(2021版)》解读[J].中华外科杂志,2022,58(4):337-342.
-
[2] Benson AB 3rd,D'Angelica MI,Abrams TA,et al.Hepatobiliary cancers,version 2.2014 [J].J Natl Compr Canc Netw,2014,12(8):1152-1182.
-
[3] Chong JU,Lee WJ.Oncologic outcomes of extended lymphadenectomy without liver resection for T1/T2 gallbladder cancer[J].Yonsei Med J,2019,60(12):1138-1145.
-
[4] Chijiwa K,Nakano K,Ueda J,et al.Surgical treatment of patients with T2 gallbladder carcinoma invading the subserosal layer [J].J Am Coll Surg,2001,192(5):600-607.
-
[5] Cho JK,Lee W,Jang JY,et al.Validation of the oncologic effect of hepatic resection for T2 gallbladder cancer:a retrospective study[J].World J Surg Oncol,2019,17(1):8.
-
[6] Choi SB,Han HJ,Kim CY,et al.Surgical outcomes and prognostic factors for T2 gallblader cancer folowing surgical resection[J].J Gastrointest Surg,2010,14(4):668-678.
-
[7] Foster JM,Hoshi H,Gibbs JF,et al.Gallbladder cancer:Defining the indications for primary radical resection and radical re-resection[J].Ann Surg Oncol,2007,14(2):833-840.
-
[8] Jung W,Jang JY,Kang MJ,et al.Effects of surgical methods and tumor location on survival and recurrence patterns after curative resection in patients with T2 gallbladder cancer [J].Gut Liver,2016,10(1):140-146.
-
[9] Kim WJ,Lim TW,Park PJ,et al.Clinicopathological differences in T2 gallbladder cancer according to tumor location [J].Cancer Control,2020,27(1):1073274820915514.
-
[10] Kwon W,Kim H,Han Y,et al.Role of tumour location and surgical extent on prognosis in T2 gallbladder cancer:an international multicentre study[].Br J Surg,2020,107(10):1334-1343.
-
[11] Lee HS,Choi DW,Park JY,et al.Surgical strategy for T2 gallbladder cancer according to tumor location[J].Ann Surg Oncol,2015,22(8):2779-2786.
-
[12] Lee W,Jeong CY,Jang JY,et al.Do hepatic-sided tumors require more extensive resection than peritoneal-sided tumors in patients with T2 gallbladder cancer?Results of a retrospective multicenter study[J].Surgery,2017,162(3):515-524.
-
[13] Li GY,Kim JH,Jung W,et al.Significance of hepatectomy in patients diagnosed with T2 gallbladder cancer [J].Surg Laparosc Endosc Percutan Tech,2020,30(1):35-39.
-
[14] Oh MY,Kim H,Sohn HJ,et al.Long-term oncologic outcomes for T2 gallbladder cancer according to the type of surgery performed and the optimal timing for sequential extended cholecystectomy[J].J Gastrointest Surg,2022,26(8):1705-1712.
-
[15] Park YJ,Hwang S,Kim KH,et al.Prognosis of patients with pT1b/T2 gallbladder carcinoma who have undergone laparoscopic cholecystectomy as an initial operation [J].Korean J Hepatobiliary Pancreat Surg,2013,17(3):113-117.
-
[16] Shindoh J,de Aretxabala X,Aloia TA,et al.Tumor location is a strong predictor of tumor progression and survival in T2 gallbladder cancer:an international multicenter study [J].Ann Surg,2015,261(4):733-739.
-
[17] Shirai Y,Yoshida K,Tsukada K,et al.Inapparent carcinoma of the gallbladder.An appraisal of a radical second operation after simple cholecystectomy[J].Ann Surg,1992,215(4):326-331.
-
[18] Sung MK,Lee W,Lee JH,et al.Comparing survival rate and appropriate surgery methods according to tumor location in T2 gallbladder cancer[J].Surg Oncol,2022,40:101693.
-
[19] Toyonaga T,Chijiwa K,Nakano K,et al.Completion radical surgery after cholecystectomy for accidentally undiagnosed gallbladder carcinoma[J].World J Surg,2003,27(3):266-271.
-
[20] Wakai T,Shirai Y,Yokoyama N,et al.Depth of subserosal invasion predicts long-term survival after resection in patients with T2 gallbladder carcinoma [J].Ann Surg Oncol,2003,10(4):447-454.
-
[21] Wright BE,Lee CC,Iddings DM,et al.Management of T2 gallbladder cancer:are practice patterns consistent with national recommendations?[J].Am J Surg,2007,194(6):820-825.
-
[22] Yokomizo H,Yamane T,Hirata T,et al.Surgical treatment of PT2 gallbladder carcinoma:a reevaluation of the therapeutic effect of hepatectomy and extra hepatic bile duct resection based on the long-term outcome[J].Ann Surg Oncol,2007,14(4):1366-1373.
-
[23] 侯纯升,徐智,张同琳,等.手术方式与T2期胆囊癌预后的关系[J].中华普通外科杂志,2006,21(12):845-847.
-
[24] Giannis D,Cerullo M,Moris D,et al.Validation of the 8th edition American joint commission on cancer(AJCC)gallbladder cancer staging system:prognostic discrimination and identification of key predictive factors[J].Cancers,2021,13(3):547.
-
[25] Al raw ash deh W,Kamarajah SK,Gujuri RR,et al.Systematic review and meta-analysis of survival outcomes in T2a and T2b gallbladder cancers[J].HPB,2022,24(6):789-796.
-
[26] Khan SM,Emile SH,Choudhry MS,et al.Tumor location and concurrent liver resection,impact survival in T2 gallbladder cancer:a meta-analysis of the literature [J].Updat Surg,2021,73(5):1717-1726.
-
[27] 冯健,张航宇,梁斌,等.胆囊癌手术治疗及预后相关因素分析[J].中华肝脏外科手术学电子杂志,2021,10(2):153-157.
-
[28] Han HS,Yoon YS,Agarwal AK,et al.La paros co pic surgery for gallbladder cancer:an expert consensus statement [J].Dig Surg,2019,36(1):1-6.
-
摘要
目的:通过Meta分析研究肝切除术对于T2期胆囊癌患者预后的影响。方法:检索Pubmed、Embase、Web of Science、Cochrane Library、中国知网、万方、维普网站。英文检索词汇包括:gallbladder carcinoma, surgery,cholecystectomy,radical cholecystectomy,hepatectomy,liver resection。中文检索词汇包括:胆囊癌、手术、胆囊切除术、根治性胆囊切除、肝切除。比较两组患者的总体生存率、无病生存率、术后并发症和术后 30 d死亡率。使用 RevMan 5.4统计软件对数据进行 Meta分析。结果:共有20个研究包含3222例患者被纳入,其中1959例患者进行了肝切除,1263例未进行肝切除。Meta分析结果显示,肝切除组与非肝切除组患者术后总生存率[风险比(RR)=0.93,95%CI:0.77~1.12,P=0.44],术后无病生存率(RR=1.11,95%CI:0.84~1.47,P=0.45),术后并发症发生率(RR=2.00,95%CI:0.71~5.62,P=0.19)及术后30 d内死亡率(RR=0.90,95%CI:0.10~8.02,P=0.92)均无显著统计学差异。结论:对于T2期胆囊癌的患者,并不能从肝切除术中获益。
Abstract
Objective To investigate the impact of hepatectomy on the prognosis of patients with T2 stage gallbladder cancer through Meta-analysis. Methods Databases including PubMed, Embase, Web of Science,Cochrane Library, CNKI, Wanfang Database, and VIP Database were searched. The search terms included:gallbladder carcinoma, surgery, cholecystectomy, radical cholecystectomy, hepatectomy, liver resection.Comparative analysis was conducted on indicators such as overall survival, disease -free survival, postoperative complication rate, and mortality within 30 days after surgery between the hepatectomy group and the non -hepatectomy group. Meta-analysis was performed using RevMan 5.4 software. Results A total of 20 studies involving 3222 patients were included, with 1959 patients in the hepatectomy group and 1263 patients in the non-hepatectomy group. Meta-analysis results showed no significant statistical differences in postoperative overall survival rate (RR=0.93, 95%CI: 0.77-1.12,P=0.44), postoperative disease-free survival rate (RR=1.11, 95%CI:0.84-1.47,P=0.45), postoperative complication rate (RR=2.00,95%CI:0.71-5.62 , P =0.19, and mortality within 30 days after surgery (RR=0.90,95%CI: 0.10-8.02,P=0.92) between the hepatectomy group and the non -hepatectomy group. Conclusion Hepatectomy does not benefit patients with T2 stage gallbladder cancer.