-
乳腺癌是乳腺上皮细胞在多种致癌因子的作用下发生增殖失控的现象,早期乳腺癌症状以乳房肿块、乳房皮肤异常、乳头溢液为主,晚期可发生淋巴结转移甚至多器官病变。临床常用的治疗方法包括手术、化疗、放疗及靶向治疗,但因癌细胞扩散,术后还会出现淋巴结转移及复发等情况,严重威胁患者生命健康[1-3]。是否发生淋巴结转移是影响乳腺癌治疗方法选择的重要因素,因此,早期检测乳腺癌患者是否出现淋巴结转移显得尤为重要。近年来,对于血清胰岛素样生长因子-1(IGF-1)、肝细胞生长因子(HGF)、肿瘤间质比值(TSR)与乳腺癌中雌激素关系的研究较多,其中血清IGF-1是一种在分子结构上与胰岛素类似的多肽蛋白物质[4]。HGF是一种可调节多种细胞生长、运动和形态发生的多功能因子[5]。TSR是影响多种癌症预后的独立危险因子[6]。IGF-1、HGF、TSR与乳腺癌肿瘤细胞活性有关,但IGF-1、HGF、TSR与乳腺癌淋巴结转移的关系还不明确。本研究旨在探究 IGF-I、HGF 与 TSR 联合检测评估乳腺癌患者淋巴结转移的价值及与预后的关系。
-
1 资料与方法
-
1.1 一般资料
-
采取回顾性研究方法,选取2015年6月—2017年8月北京市通州区妇幼保健院乳腺科收治的120例乳腺癌患者作为研究对象,根据手术后病理学结果患者是否发生淋巴结转移将其分为复发转移组24例、未复发转移组96例。纳入标准:1)患者年龄35~65岁;2)乳腺癌的诊断标准参考《中国抗癌协会乳腺癌诊治指南与规范》2021版中的标准[7];3)乳腺癌及淋巴结转移情况均经过病理学检查证实;4)患者于手术前接受了相关检查;5)患者均至少接受了60个月的随访观察,记录患者肿瘤复发、转移及生存情况。排除标准:1)既往手术后复发的乳腺癌患者;2)预计生存期不足3个月;3)合并严重的系统疾病(如脑梗死、心肌梗死、重症心衰、严重的感染疾病等);4)合并有其他部位的恶性肿瘤。本研究方案符合我院医学伦理委员会规定(审批号:2022-TZFY-015-01)。
-
1.2 酶联免疫吸附试验检查IGF-1、HGF、TSR水平
-
采集患者清晨空腹新鲜血液标本5 mL,使用转速为1000 r/min的离心机,离心半径为10 cm,离心处理20 min,分离血清,采用酶联免疫吸附试验试剂盒(苏州博园医疗科技有限公司)检测血清IGF-1、HGF及TSR水平。
-
1.3 统计学方法
-
数据用SPSS 24.0软件处理,IGF-1、HGF、TSR等计量资料采用进行统计描述,两组间差异检验采用独立样本t检验;计数资料(TNM分期、组织学分级、病灶大小等)用例(%)描述,组间对比分析用χ2检验;IGF-1、HGF、TSR在诊断乳腺癌发生淋巴结转移采用受试者工作特征曲线(ROC)分析;最后采用多因素Logistic回归模型分析乳腺癌转移复发的危险因素;P<0.05为差异有统计学意义。
-
2 结果
-
2.1 两组的IGF-1、HGF、TSR水平比较
-
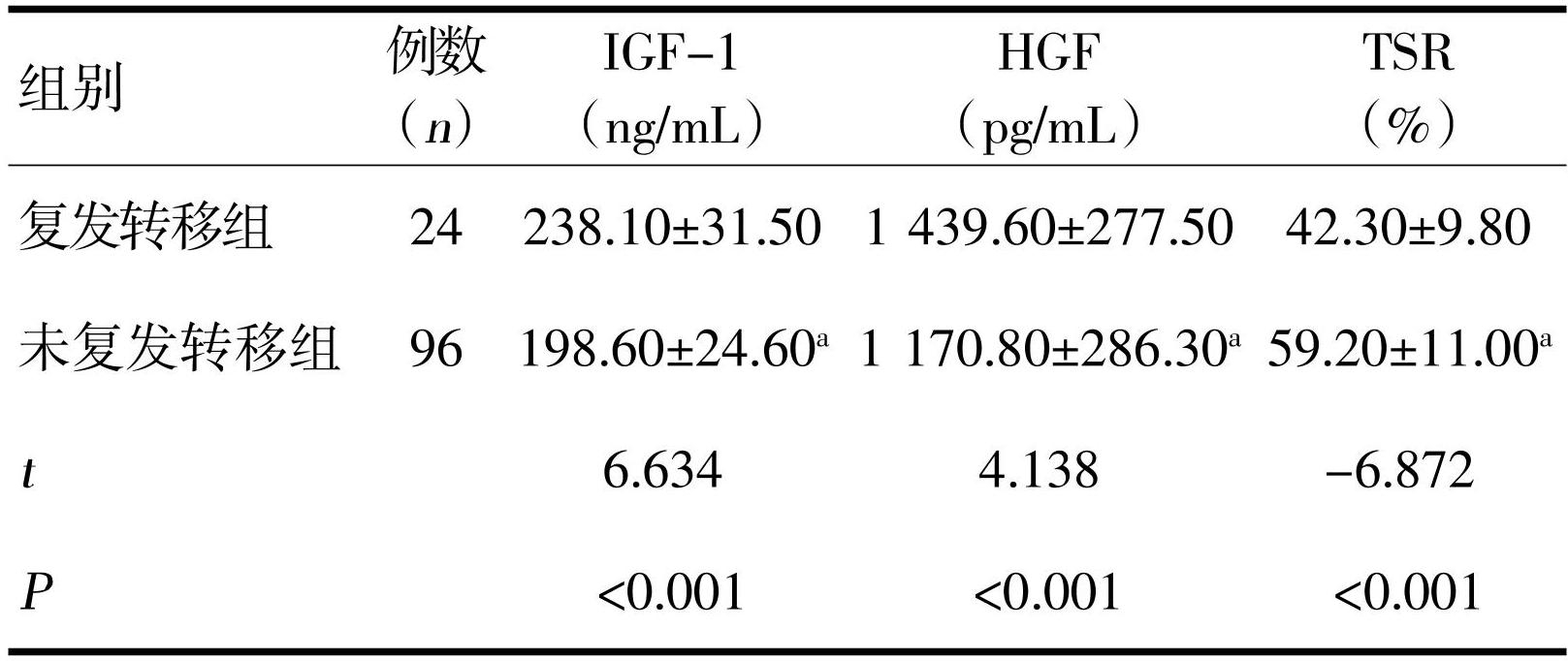
乳腺癌淋巴结转移组患者的IGF-1、HGF水平高于非转移组,TSR水平低于非转移组,差异均有统计学意义(P<0.05),表1。
-
注: a与转移组比较,P<0.05
-
2.2 IGF-1、HGF、TSR在乳腺癌发生淋巴结转移中的诊断价值
-
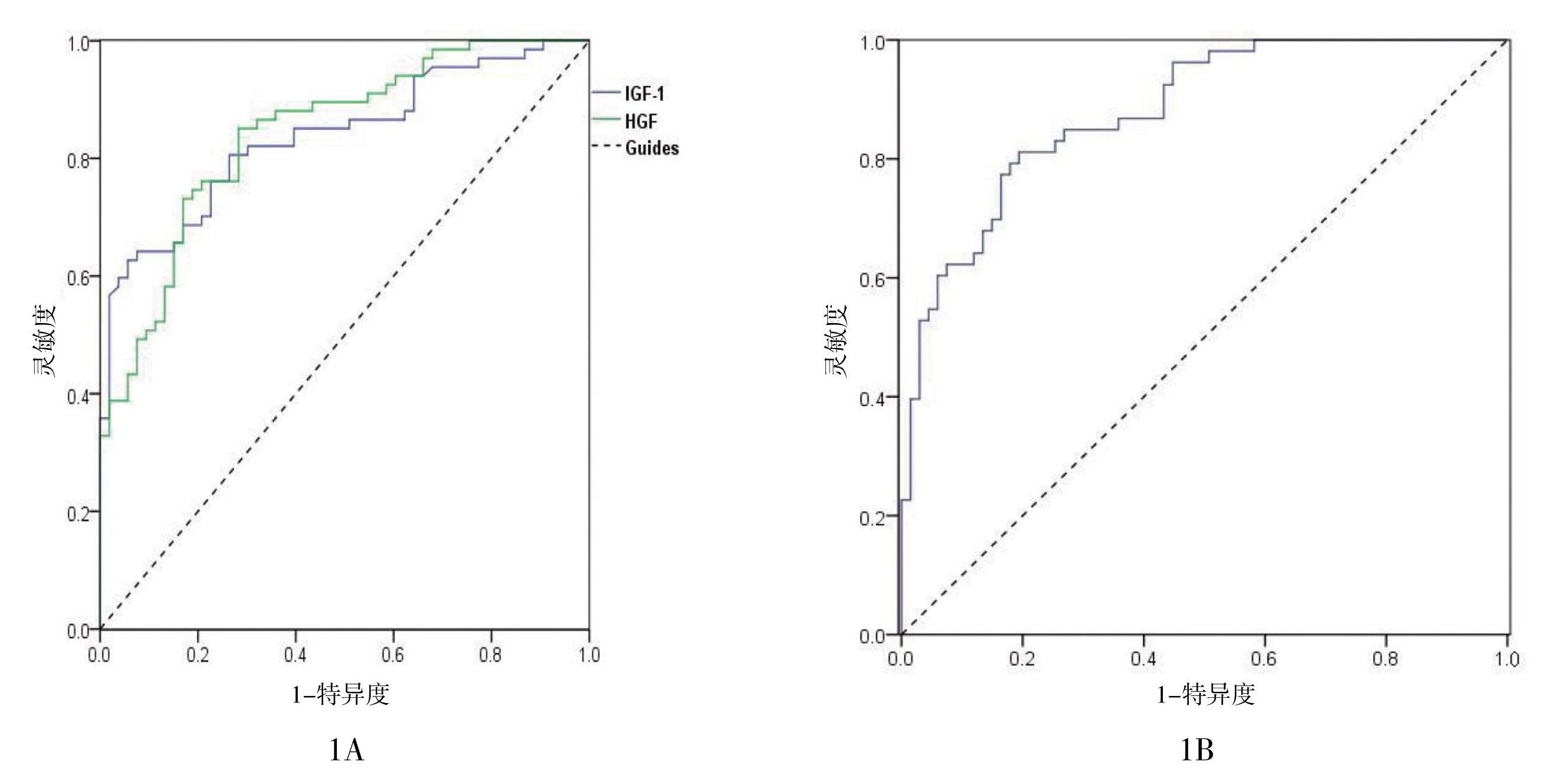
以IGF-1、HGF、TSR检查结果分别绘制ROC曲线,IGF-1、HGF、TSR诊断乳腺癌发生淋巴结转移的ROC曲线下面积(AUC)值分别为0.837(0.766~0.907)、0.842(0.773~0.911)、0.880(0.821~0.938),见图1。
-
2.3 乳腺癌转移复发的单因素风险分析
-
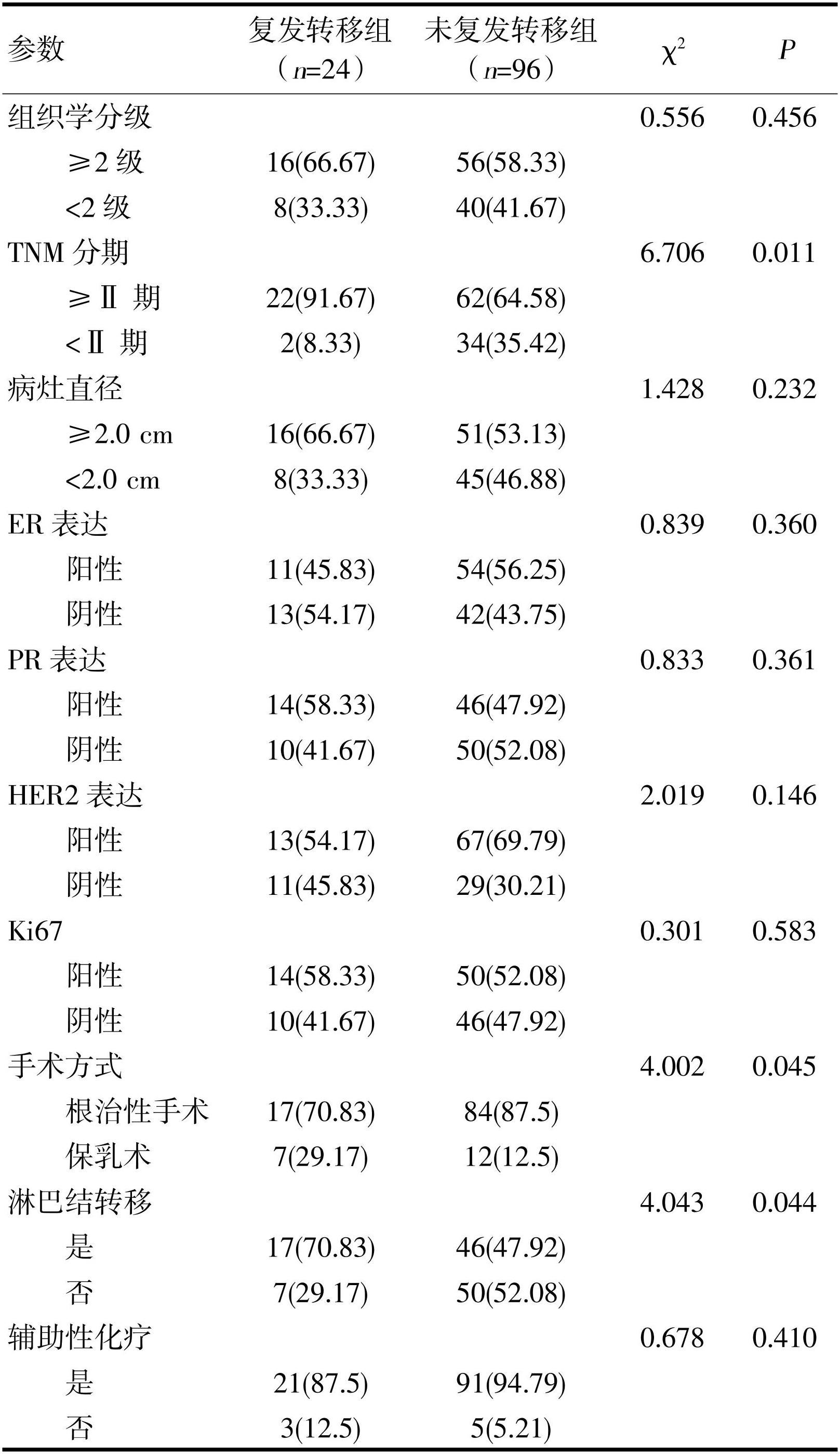
对比24例出现术后复发转移的乳腺癌与96例未出现复发转移的乳腺癌患者的病理学及治疗指标,复发转移组TNM分期中≥Ⅱ期患者占比、淋巴结转移阳性患者占比、保乳手术患者占比均高于未复发转移组,差异有统计学意义(P<0.05),表2。
-
图1 IGF-1、HGF(1A)及TSR(1B)诊断乳腺癌发生淋巴结转移的ROC曲线
-
2.4 乳腺癌患者转移复发的多因素Logistic回归分析
-
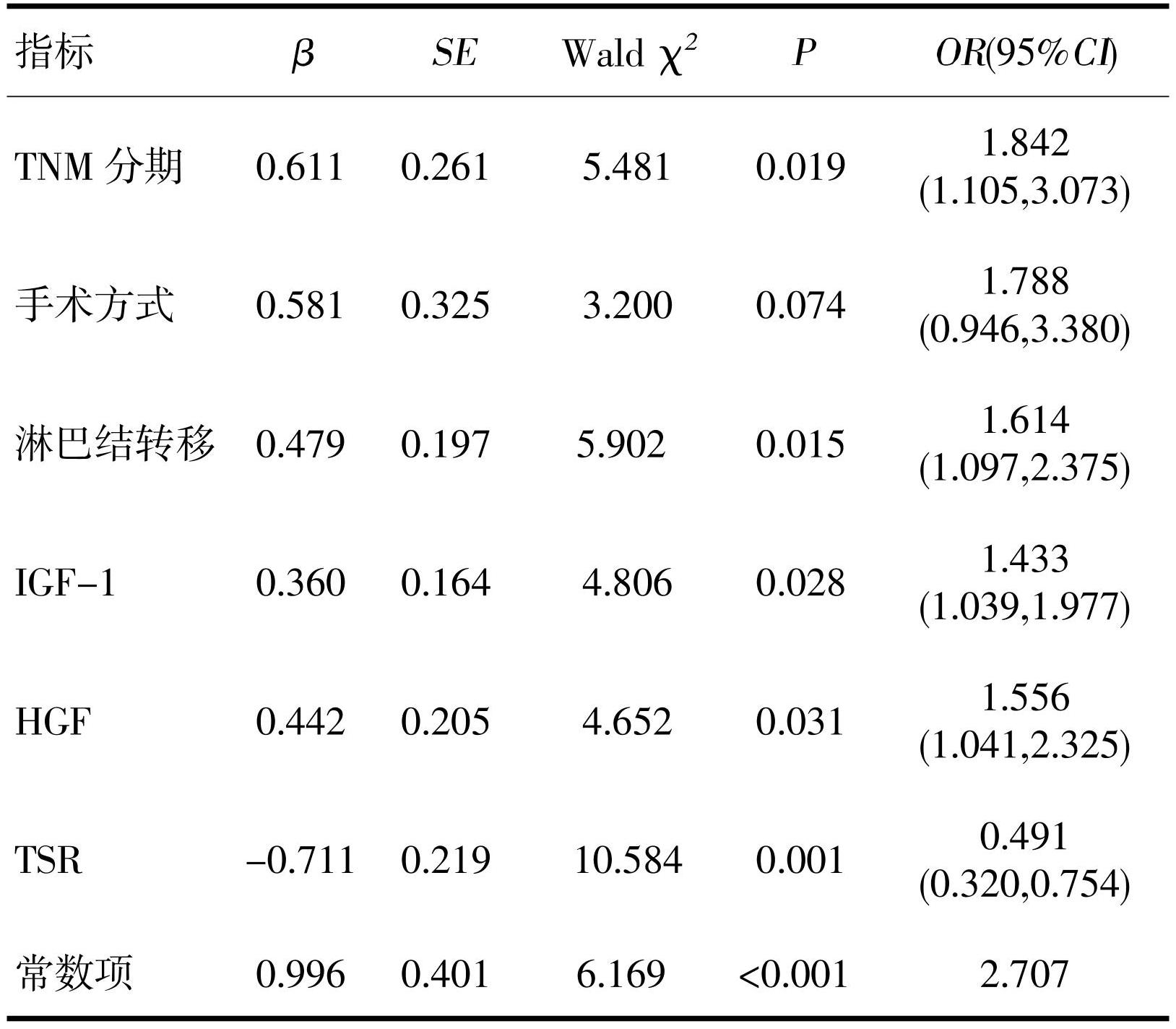
以上述各项单因素分析具有统计学差异的TNM分期中、手术方式、是否发生淋巴结转移、IGF-1、HGF、TSR测定值作为自变量,以患者5年随访结局作为因变量,建立Logistic回归模型,结果显示:TNM分期≥Ⅱ期、发生淋巴结转移、IGF-1水平增高、HGF水平增高、TSR低水平会增大乳腺癌患者手术治疗后复发转移的风险(P<0.05),表3。
-
3 讨论
-
近年来对于血清IGF-1、HGF、TSR等多种内源性激素对乳腺癌患者癌细胞扩散的研究较多[8-10]。其中血清IGF-1是是一类多功能细胞增殖调控因子,HGF肝细胞生长因子是重要的抗纤维化因子,能修复受损肺组织,是重要的保护性因子[11]。TSR指肿瘤组织内肿瘤细胞与间质部分的比例。有研究表示IGF-1、HGF、TSR对乳腺癌细胞扩散相关[12]。但对与乳腺癌出现淋巴结转移的研究尚少,故本研究采用IGF-1、HGF、TSR对乳腺癌出现淋巴结转移进行诊断。
-
本研究对两组患者IGF-1、HGF、TSR检查结果进行比较,结果显示转移组患者IGF-1、HGF水平显著高于非转移组,TSR水平明显低于非转移组,表明IGF-1、HGF、TSR水平与乳腺癌是否发生淋巴结转移相关。已有研究证实,乳腺癌中存在IGF-1异常表达[13]。IGF-1浓度由包括胰岛素样生长因子结合蛋白-3(IGFBP-3)在内的结合蛋白控制,淋巴结转移会出现大量癌细胞增殖分化,促使IGF-1增殖分化,且有研究表示,IGF-1与乳腺癌淋巴结转移具有相关性[14]。HGF是一种血源性生长因子,当淋巴结转移时,HGF由间充质细胞分泌水解生成α和β链,形成成熟异二聚体,可促进人体淋巴管形成,同时造成血管内皮细胞增殖[15-16]。TSR是肿瘤组织内肿瘤细胞和间质细胞的比值,乳腺癌出现淋巴结转移,说明病情逐渐加重,肿瘤细胞以及间质细胞增加,从而导致TSR比值增加[17]。因此,IGF-1、HGF、TSR可以评估是否发生淋巴结转移。
-
本研究结果显示IGF-1、HGF、TSR诊断乳腺癌淋巴结转移的ROC曲线下面积分别为0.837、0.842、0.880,表明三者的诊断价值均较好,进一步提示IGF-1、HGF、TSR可作为评估乳腺癌发生淋巴结转移的有效指标。有研究发现,IGF-1、HGF可作为血清指标预测乳腺癌患者是否发生淋巴结转移[18-20],与本研究结果基本一致。同时TSR能够反映乳腺癌周围肿瘤细胞和间质细胞数量,可独立使用预测肿瘤预后[21-23]。本研究结果显示TSR在淋巴结转移时异常表达,进一步印证了TSR与乳腺癌淋巴结转移的相关性。本研究结果显示转移组复发转移率和未复发转移率明显高于非转移组,表明乳腺癌发生淋巴结转移术后复发率高。淋巴结转移情况与原发肿瘤大小有关,肿瘤体积越大,腋淋巴结转移率越高,转移数越多[24-26]。由于乳腺深部淋巴网可与腹直肌鞘和肝镰状韧带的淋巴管相通,从而使乳腺深部的淋巴结转移到向肝脏,而当正常淋巴途径梗阻时,癌细胞会经内乳淋巴链逆流至肝脏[27-29]。因此,存在淋巴结转移的乳腺癌复发率高。
-
本研究对乳腺癌转移复发的单因素风险进行分析,结果显示复发转移组患者的TNM分期中≥Ⅱ期患者占比、保乳手术患者占比均高于未复发转移组患者,表明存在淋巴结转移的乳腺癌肿瘤进展程度比较高。进一步进行多因素分析,结果显示TNM分期≥Ⅱ期、发生淋巴结转移、IGF-1水平增高、HGF水平增高、TSR低水平会增大乳腺癌患者手术治疗后复发转移的风险,表明TNM分期≥Ⅱ期、淋巴结转移以及IGF-1、HGF、TSR水平可以预测乳腺癌患者手术预后情况。有研究表示,TNM分期对于预测肿瘤复发转移价值不可低估,是临床上比较成熟的风险评估指标[30-32]。而当乳腺癌出现淋巴结转移,说明乳腺癌已处于晚期状态,预后较差[33-35]。同时上述结果已经证明IGF-1、HGF、TSR水平可作为乳腺癌术后复发转移的有效指标。因此本研究结果进一步被证实。
-
本研究分析了IGF-1、HGF、TSR与乳腺癌患者淋巴结转移和预后的关系,为今后的研究提供了有价值的参考。但本研究中未对不同病理类型的乳腺癌进行单独分析,在后续研究中还需要进一步细化乳腺癌的病理分型,分析上述指标与不同病理类型乳腺癌淋巴结转移和预后的关系。
-
综上所述,IGF-1、HGF水平增高及TSR降低会增大乳腺癌患者发生手术后复发的风险,术前检查IGF-1、HGF及TSR在可以评估是否发生淋巴结转移,对手术方案制定有一定的参考价值。
-
参考文献
-
[1] Noguchi M,Inokuchi M,Noguchi M,et al.Axillary surgery for breast cancer:past,present,and future[J].Breast Cancer,2021,28(1):9-15.
-
[2] Lin AP,Huang TW,Tam KW.Treatment of male breast cancer:meta-analysis of real-world evidence[J].Br J Surg,2021,108(9):1034-1042.
-
[3] Chang JM,Leung JWT,Moy L,et al.Axillary nodal evaluation in breast cancer:state of the art[J].Radiology,2020,295(3):500-515.
-
[4] 邢海霞,赵明燕,郭勇.乳腺癌患者血清性激素、IGF-1、VEGF和组织LOX水平与淋巴结转移的相关性分析[J].分子诊断与治疗杂志,2019,11(2):122-127.
-
[5] 刘海旺,张宏旭,刘燃,等.HGF、E-cad蛋白在乳腺癌组织中的表达及其临床意义[J].解放军预防医学杂志,2019,37(12):7-8.
-
[6] Song BI.A machine learning-based radiomics model for the prediction of axillary lymph-node metastasis in breast cancer[J].Breast Cancer,2021,28(3):664-671.
-
[7] 中国抗癌协会乳腺癌专业委员会.中国抗癌协会乳腺癌诊治指南与规范(2021年版)[J].中国癌症杂志,2021,31(10):954-1040.
-
[8] To B,Isaac D,Andrechek ER.Studying lymphatic metastasis in breast cancer:current models,strategies,and clinical perspectives[J].J Mammary Gland Biol Neoplasia,2020,25(3):191-203.
-
[9] Hetterich M,Gerken M,Ortmann O,et al.Adjuvant chemotherapy for breast cancer patients with axillary lymph node micrometastases[J].Breast Cancer Res Treat,2021,187(3):715-727.
-
[10] Veronesi P,Ghidinelli F,Corso G.Axillary surgery in breast cancer:evolution and de-escalation[J].Minerva Chir,2020,75(6):383-385.
-
[11] 庄晓苹,林琼琼,季剑乐,等.乳腺癌中SyK、HGF表达的相关性及预后的关系[J].医学研究杂志,2019,48(5):126-129.
-
[12] Arjmandi F,Mootz A,Farr D,et al.New horizons in imaging and surgical assessment of breast cancer lymph node metastasis[J].Breast Cancer Res Treat,2021,187(2):311-322.
-
[13] Montagna G,Corso G,Di Micco R,et al.Axillary management after neoadjuvant treatment[J].Minerva Chir,2020,75(6):400-407.
-
[14] Bordea C,Gherghe M,Capsa C,et al.Sentinel lymph node biopsy after neoadjuvant treatment for breast cancer.the validation protocol[J].Chirurgia(Bucur),2021,116(2):178-185.
-
[15] Braunstein LZ,Bellon JR.Contemporary issues in breast cancer radiotherapy[J].Oncol Clin N Am,2020,34(1):1-12.
-
[16] Yamashita Y,Tsunoda H,Nozaki F,et al.Evaluation of axillary lymph nodes in breast cancer patients with atopic dermatitis[J].Ultrasound Med Biol,2021,47(3):370-375.
-
[17] Euhus DM.Management of the clinically positive axilla[J].Breast J,2020,26(1):35-38.
-
[18] Costaz H,Rouffiac M,Boulle D,et al.Stratégies en cas de positivité du ganglion sentinelle dans les cancers du sein[J].Bull Du Cancer,2020,107(6):672-685.
-
[19] Caffa I,Spagnolo V,Vernieri C,et al.Fasting-mimicking diet and hormone therapy induce breast cancer regression[J].Nature,2020,583(7817):620-624.
-
[20] Zhang Q,Li TF,Wang ZC,et al.lncRNA NR2F1-AS1 promotes breast cancer angiogenesis through activating IGF-1/IGF-1R/ERK pathway[J].J Cell Mol Med,2020,24(14):8236-8247.
-
[21] Murphy N,Knuppel A,Papadimitriou N,et al.Insulin-like growth factor-1,insulin-like growth factor-binding protein-3,and breast cancer risk:observational and Mendelian randomization analyses with ∼430 000 women[J].Ann Oncol,2020,31(5):641-649.
-
[22] Biro FM,Huang B,Wasserman H,et al.Pubertal growth,IGF-1,and windows of susceptibility:puberty and future breast cancer risk[J].J Adolesc Health,2021,68(3):517-522.
-
[23] Tin ST,Reeves GK,Key TJ.OP47 Endogenous hormones and risk of invasive breast cancer in pre-and post-menopausal women:findings from the UK biobank[C]//SSM Annual Scientific Meeting.BMJ Publishing Group Ltd,2021,125(1):126-134.
-
[24] Wu XY,Zhang XF,Hao Y,et al.Obesity-related protein biomarkers for predicting breast cancer risk:an overview of systematic reviews[J].Breast Cancer,2021,28(1):25-39.
-
[25] Costa-Silva DR,da Conceição Barros-Oliveira M,da Silva BB.Systematic review of insulin-like growth factor 1 gene expression in women with breast cancer[J].Rev Assoc Med Bras,2021,67(9):1372-1376.
-
[26] Alkhayyal N,Talaat I,Vinodnadat A,et al.Correlation of insulin-like growth factor 1 receptor expression with different molecular subtypes of breast cancer in the UAE[J].Anticancer Res,2020,40(3):1555-1561.
-
[27] Mahsa,Lahiji R,.The effect of synbiotic on glycemic profile and sex hormones in overweight and obese breast cancer survivors following a weight-loss diet:a randomized,triple-blind,controlled trial[J].Clin Nutr,2021,40(2):394-403.
-
[28] Jones GS,Hoadley KA,Benefield H,et al.Racial differences in breast cancer outcomes by hepatocyte growth factor pathway expression[J].Breast Cancer Res Treat,2022,192(2):447-455.
-
[29] Millar R,Kilbey A,Remak SJ,et al.The MSP-RON axis stimulates cancer cell growth in models of triple negative breast cancer[J].Mol Oncol,2020,14(8):1868-1880.
-
[30] Vrabie EM,Alecu M,Cirimbei C,et al.The management of axillary lymph nodes in breast cancer-A retrospective single-centre study[J].Chirurgia,2021,116(2):186-192.
-
[31] Lin Y,Xu Y,Wang CJ,et al.Loco-regional therapy and the risk of breast cancer-related lymphedema:a systematic review and meta-analysis[J].Breast Cancer,2021,28(6):1261-1272.
-
[32] Ditsch N,Rubio IT,Gasparri ML,et al.Breast and axillary surgery in malignant breast disease:a review focused on literature of 2018 and 2019[J].Curr Opin Obstet Gynecol,2020,32(1):91-99.
-
[33] Baran M,Ozturk F,Canoz O,et al.The effects of apoptosis and apelin on lymph node metastasis in invasive breast carcinomas[J].Clin Exp Med,2020,20(4):507-514.
-
[34] Ramdani H,El Haddad S,Chat L,et al.Axillary schwannoma mimicking a breast cancer lymph node metastasis[J].Breast J,2021,27(4):387-388.
-
[35] Liu JL,Chen DS,Cheng Z,et al.Expression of SOX10 and GATA3 in breast cancer and their significance[J].Zhonghua Bing Li Xue Za Zhi,2022,51(6):536-541.
-
摘要
目的:探讨血清胰岛素样生长因子-1(IGF-1)、肝细胞生长因子(HGF)、肿瘤间质比值(TSR)诊断乳腺癌发生淋巴结转移的价值及与患者预后的关系。方法:采取回顾性研究方法,选取2015年6月—2017年8月北京市通州区妇幼保健院乳腺科收治的120例乳腺癌患者作为研究对象,根据手术后病理学结果患者是否发生淋巴结转移将其分为复发转移组24例、未复发转移组96例,对比两组患者的血清IGF-1、HGF、TSR值,采用受试者工作曲线分析三项指标诊断乳腺癌患者发生淋巴结转移的价值;采用Logistic回归模型分析乳腺癌病理学特征、治疗方法及IGF-1、HGF、TSR与乳腺癌患者预后结局的关系。结果:乳腺癌淋巴结转移组患者的IGF-1、HGF测定值高于非转移组,TSR水平低于非转移组,差异均有统计学意义(P<0.05);IGF-1、HGF、TSR测定值诊断乳腺癌发生淋巴结转移的ROC曲线下面积值分别为0.837(0.766~0.907)、0.842(0.773~0.911)、0.880(0.821~0.938);Logistic回归分析结果显示:TNM分期≥Ⅱ期、发生淋巴结转移、IGF-1水平增高、HGF水平增高、TSR低水平会增大乳腺癌患者手术治疗后复发转移的风险(P<0.05)。结论:IGF-1、HGF水平增高及TSR降低会增大乳腺癌患者发生手术后复发的风险,术前检查IGF-1、HGF及TSR可以评估是否发生淋巴结转移,对手术方案制定有一定的参考价值。
Abstract
Objective To investigate the value of serum insulin-like growth factor-1 (IGF-1), hepatocyte growth factor (HGF) and tumor stroma ratio (TSR) in the diagnosis of lymph node metastasis in breast cancer and their relationship with prognosis. Methods A retrospective study was conducted to select 120 patients with breast cancer who were admitted to the Breast Department of Tongzhou District Maternal and Child Health Hospital from June 2015 to August 2017 as the study subjects. According to the pathological results after surgery, the patients were divided into 24 patients with recurrent metastasis and 96 patients without recurrent metastasis, and the serum IGF-1, HGF, TSR values of the two groups were compared, The value of three indicators in the diagnosis of lymph node metastasis in breast cancer patients was analyzed by subject work curve; Logistic regression model was used to analyze the relationship between the pathological characteristics, treatment methods, IGF-1, HGF, TSR and the prognosis of breast cancer patients. Results IGF-1 and HGF in patients with lymph node metastasis of breast cancer were significantly higher than those in patients without metastasis, and TSR in patients with breast cancer metastasis was significantly lower than those in patients without metastasis (P<0.05); The AUC values under the ROC curve of IGF-1, HGF and TSR for diagnosis of lymph node metastasis in breast cancer were 0.837 (0.766-0.907), 0.842 (0.773-0.911) and 0.880 (0.821-0.938), respectively; Logistic regression model: TNM stage ≥ stage II, lymph node metastasis, elevated IGF-1 level, elevated HGF level, and low TSR level will increase the risk of recurrence and metastasis of breast cancer patients after surgery (P<0.05). Conclusion The increase of IGF-1, HGF and TSR levels and the decrease of TSR will increase the risk of postoperative recurrence in breast cancer patients. Preoperative examination of IGF-1, HGF and TSR can evaluate whether lymph node metastasis occurs, which has certain reference value for the formulation of surgical plan.